From paracetomol to transcranial magnetic stimulation, everything I know so far about pain in MS.
I’m not going to pretend to know everything about this huge topic, but here is my best shot at present! I started putting the info together for a presentation for MS specialists, with anaesthetist Dr. Sharmila Khot, and then I carried on, to try to compile all I’ve learned into a blogpost. Referenced version available on request.

Pain affects around 63% of people with MS. In a 2012 article about the types of pain in MS, the authors state ‘We can think of no other disease that can result in so manyk different types of pain.’
They list 9 types of pain in MS, as:
- Muscle spasm – (like cramp)
- Spasticity – (tight / stiff)
- Musculo-skeletal – (back or joint problems, often from walking difficulties, or sitting)
- Optic neuritis – (pain in the eye due to inflammation of the optic nerve)
- Migraine – (in fact, unless linked to beta interferon or fingolimod, MS does not cause migraine, but headaches are more common in people with MS than in the general population)
- Treatment related pain – (injectable DMTs/ side effects)
- Neuropathic pain & ongoing extremity pain – (prickling, tingling or shooting stabbing pains, and pins & needles, burning/freezing, often worst in the feet)
- Trigeminal neuralgia – (agonising bouts of facial pain)
- L’Hermittes sign – (like an electric shock when bending the head forwards)
I’d like to add to the list, the pain of fatigued muscles.
In nursing, we have a process, whose acronym is ADPIE.

Photo by Pixabay on Pexels.com
It stands for
- Assess
- Diagnose
- Plan
- Implement
- Evaluate
This process needs to go on continually, when assessing and treating pain. The first two steps, assessment and diagnosis, are essential to plan and implement the right treatment, and for this, your description of how the pain feels and when it occurs are essential.
The two broadest categories are ‘nociceptive’ (or normal type pain, which is often musculoskeletal), and ‘neuropathic’, (or nerve pain). Many people with MS have a mixture of different types of pain.
NOCICEPTIVE PAIN
Nociceptive, or normal type pain, is most likely to be described as gnawing, throbbing, aching, cramping, or dull, and in the joints, or muscles.
This includes the pain cause by muscle spasm, stiffness, or spasticity, which needs to be addressed by treating that problem; see mstrust.org.uk/a-z/spasticity-and-spasms
and Natural options for MS spasms are discussed here
Key interventions are muscle relaxants and physiotherapy.
Musculoskeletal pain is not caused by MS primarily, but it can be a secondary effect of effortful walking, using a stick, sitting for long periods, or becoming deconditioned, and cause, for instance, low back pain, shoulder pain, hip pain. Having high tone or stiffness in the muscles can contribute to this pain, so seeing one of your MS health professionals to work out how much this is contributing, and work out a treatment plan, can be helpful.
For musculoskeletal (MSK) pain, standard medical practice is exercise, physiotherapy, and painkillers.

A physiotherapist can both treat you, and advise on the best form of exercise. A good physiotherapist will also be able to detect specific painful problems that may have specific treatments. For example, Piriformis syndrome can happen to runners, but also to people who have to sit for long periods of time, so can affect wheelchair users. In Piriformis syndrome, the sciatic nerve is pinched by the small piriformis muscle in the buttock, causing horrible pain and discomfort in the buttock when sitting, and specific stretches are recommended to release it.( Post to follow)
Exercise is a cornerstone in treating musculoskeletal pain, and the most recent findings in pain science suggest that in chronic pain, doing exercise, even when it is painful to do so, can reduce pain in the long term, by reducing ‘fear avoidance’ of movement and further worsening and de-conditioning; by de-sensitising chronic pain areas which have become over sensitised; and also by stimulating the circulation of lymph and oxygen, lowering inflammation. If you have physical barriers to exercise, consider adaptive equipment – electric bikes, power assisted exercise bikes, swimming with disabled access, GP exercise referral, or MS exercise classes.
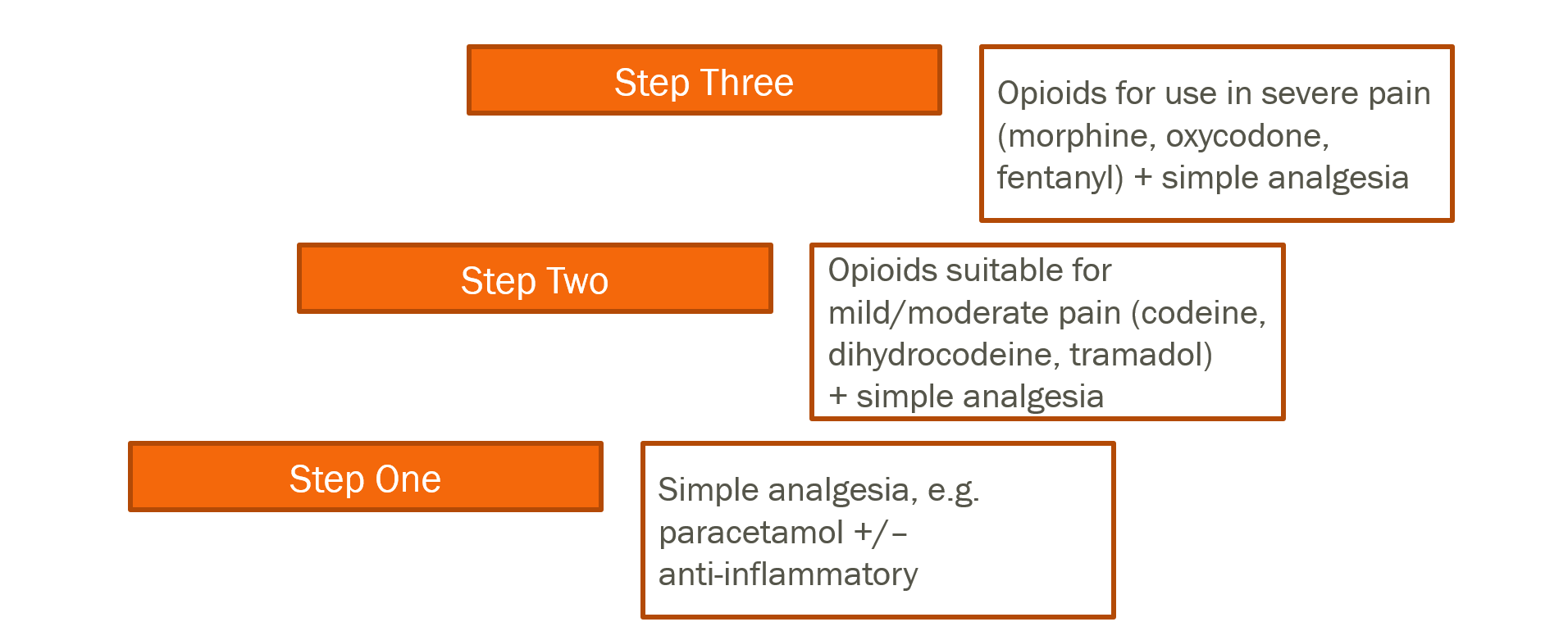
Painkillers vary in different conditions, but generally follow the World Health Organisation ladder of analgesia.
This ladder was initially put together to help cancer pain, and there is now lot of debate about how useful, or harmful, it really is to use opioids in chronic pain.
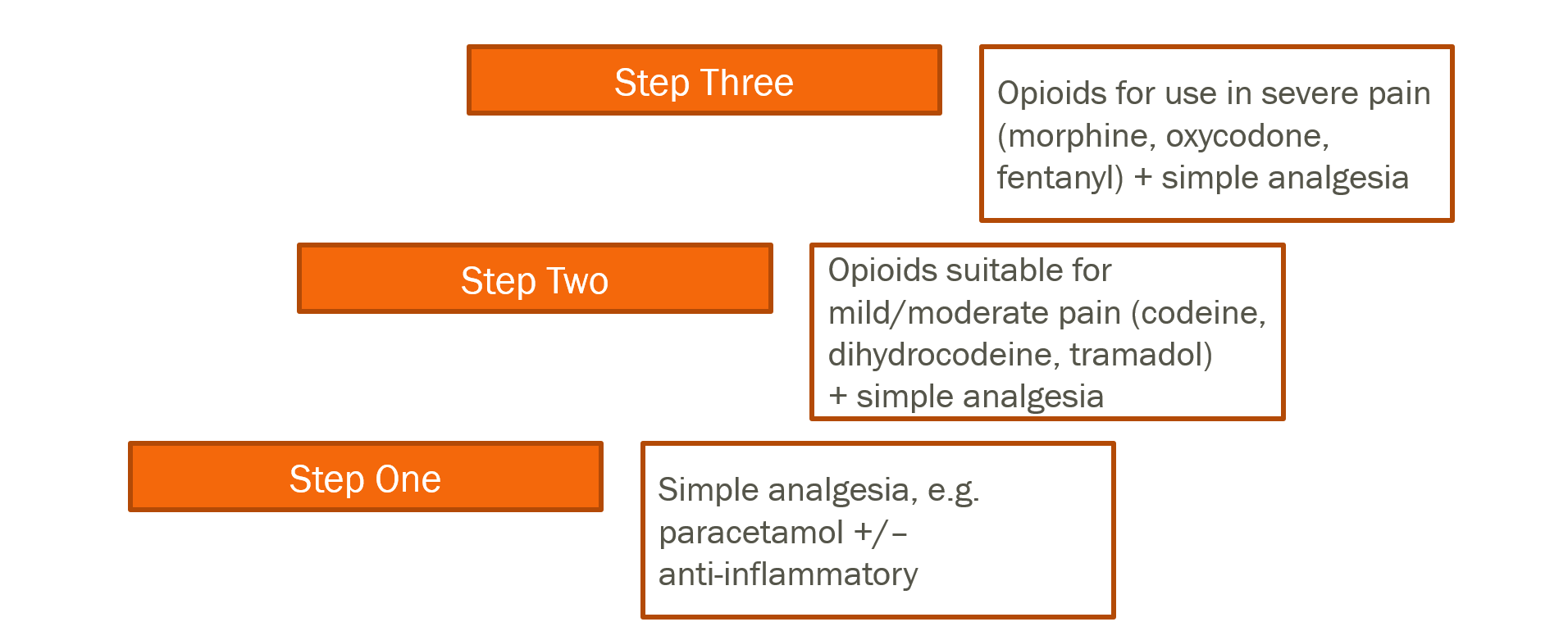
Using Opioids
There are concerns about the prescription of opioids for long term pain, due to the problems of side-effects, tolerance ( the body needing a higher and higher dose to be effective), dependence ( when the body only functions normally with the drug, and trying to cut down or withdraw from it causes unpleasant symptoms) and risk of addiction. Guidance for healthcare professionals is here: https://www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware.
In summary,
- opioids are most useful for acute pain, and end of life ( cancer type) pain
- For best results in chronic/persistent pain, they should be low dose, and used only intermittently, to prevent tolerance
- Above a dose of 120mg a day of morphine, or equlivalent, there is no increased pain relief, but increased risks
- If pain does not respond to opioids there is no benefit to taking them, and they should be stopped, but all tapering down and withdrawing needs close monitoring and support.
Gels and creams
Anti-inflammatories gels are also available, but remember that the doses count towards your daily allowance of the drug. The evidence for these is good in acute pain, but only minimal in long term pain.
Some people also find that over the counter heat rubs help; these work in a different way, as Counterirritants. Ingredients such as menthol, methylsalicylate (oil of evergreen), and camphor create a burning or cooling sensation that distracts your mind from the pain.
Salicylates. These same ingredients that give aspirin its pain-relieving quality are found in some creams. When absorbed into the skin, they may help with pain, particularly in joints.
There is less robust evidence for the above 2 topical applications.
Capsaicin cream has good evidence to support its use, and can be prescribed for both joint and neuropathic pain. It’s made from chilli peppers, and burns when it goes on, but if persisted with over weeks, can provide relief by desensitising the nerves, and I’ve occasionally seen it work when other treatments have failed!
Complementary therapies

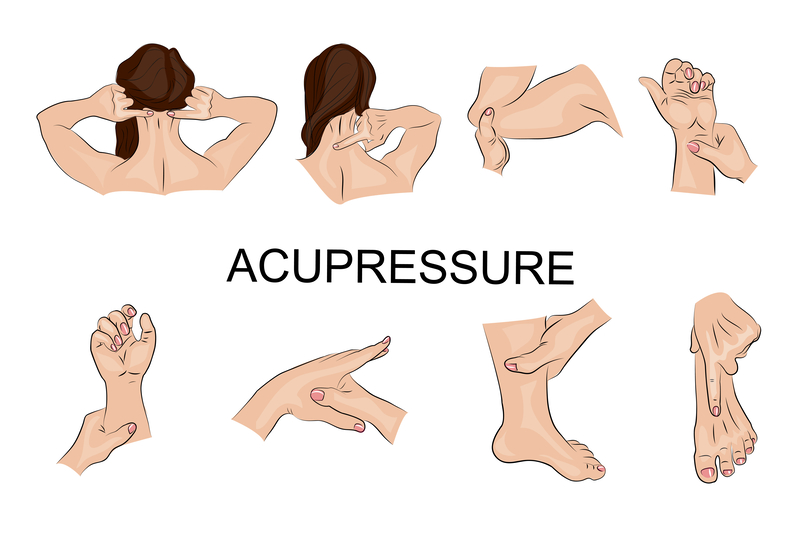
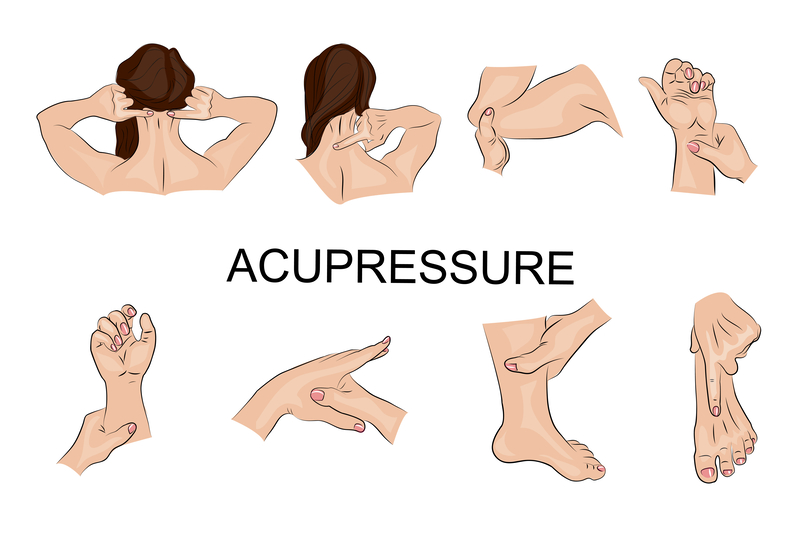
As well as standard treatments, many people with MSK pain benefit from complementary therapies, including, but not limited to, Acupuncture, Massage, Reflexology, Craniosacral, Osteopathy, Chiropractic, Bowen technique, Shiatsu and massage. The practice with the most published evidence, showing moderate but sustained benefit in one review of research, is acupuncture.
It’s worth knowing that there is a great deal of difference in the amount of training done by a traditional Chinese acupuncturist, who will have trained for many years, and the acupuncture you might receive as part of standard medical treatment, which may have been a very short course for doctors or physios.
Reflexology and acupressure work on the same principles, and acupressure is a technique you can do on yourself at home.
Electrotherapies are also often used successfully, and include many types of device, either as part of physiotherapy treatment or privately bought home use machines, and there are varying degrees of evidence for efficacy of the different types. See Electrotherapies
Also see ‘For all types of persistent pain’
NEUROPATHIC PAIN
Neuropathic, or nerve pain is caused by ‘a lesion or disease affecting the somatosensory system.’ It is commonly described as burning, hot, icy cold, tingling, pins and needles, electric shocks, shooting or stabbing.
Neuropathic pain is a difficult pain to manage, especially as it can be worse with exercise, and normal painkillers aren’t effective.
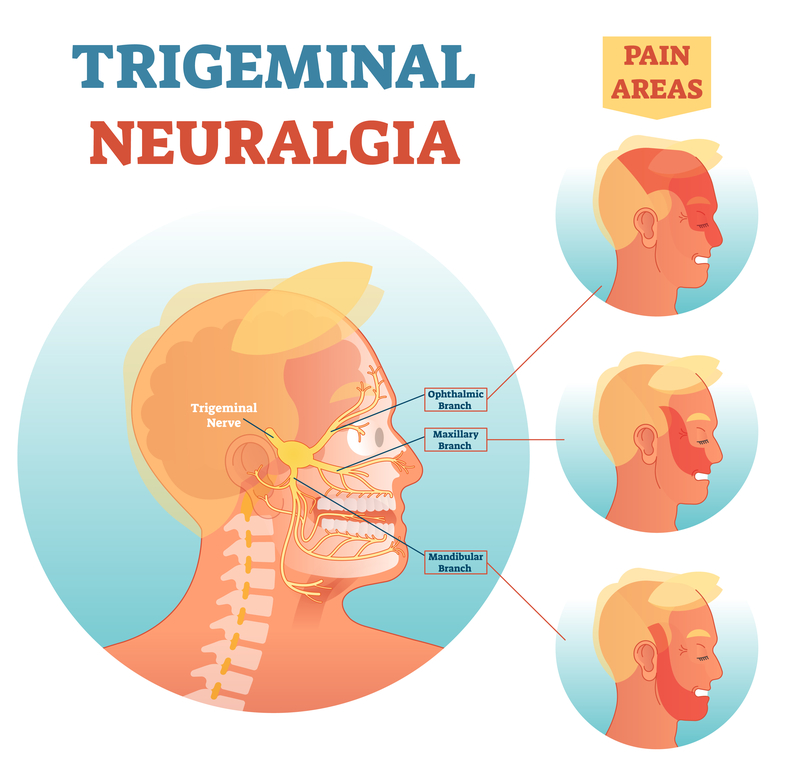
Trigeminal neuralgia is a type of neuropathic pain that is treated differently from others.
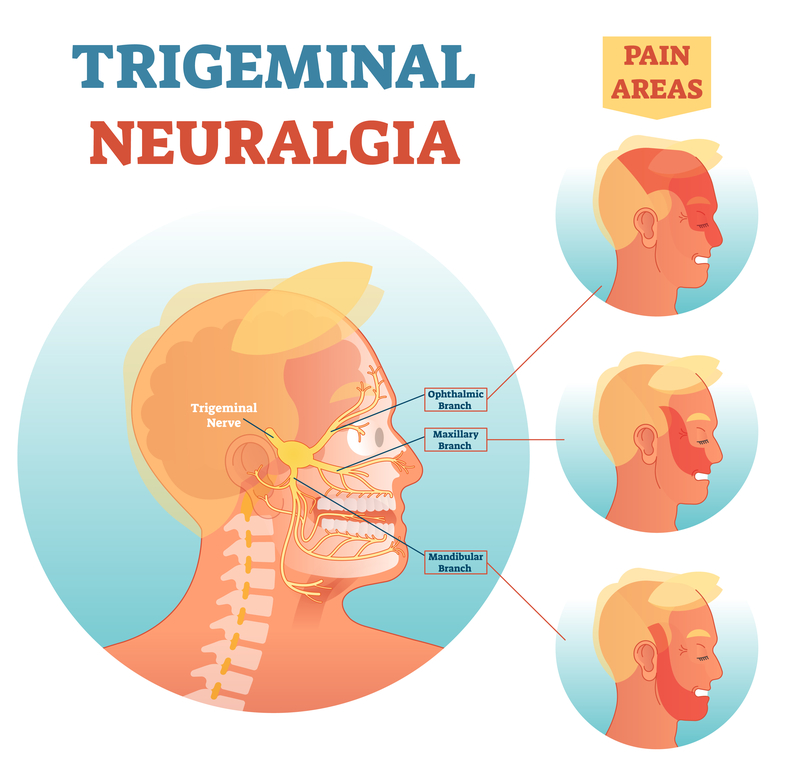
It’s is an agonizing facial pain which come in bouts, but can develop into permanent pain. This requires Carbamazepine as a firstline, but with a specialist, other medications can be tried, and there are both non-invasive and surgical procedures available. See https://www.nhs.uk/conditions/trigeminal-neuralgia/
For the other neuropathic pains,
Firstline medications
that can be prescribed in primary care ( ie by/via your GP) are in the following table. NB. Side effects are only potential side effects. ‘Common’ means between 1 in 10 and 1 in 100 people are affected.
Medication & example brand name
Description, Dose, Side effects
Only the most common side effects are listed; before recommendation or prescription, read full list of possible side effects at https://bnf.nice.org.uk/
Gabapentin (Neurontin)
Description: Antiepileptic Dose: Initially 300 mg once daily on day 1, then 300 mg twice daily on day 2, then 300 mg 3 times a day on day 3, alternatively initially 300 mg 3 times a day on day 1, then increased in steps of 300 mg every 2–3 days in 3 divided doses, adjusted according to response; maximum 3.6 g per day.
Common side effects: Anxiety; appetite abnormal; arthralgia; asthenia; behaviour abnormal; confusion; constipation; cough; depression; diarrhoea; dizziness; drowsiness; dry mouth; dysarthria; dyspnoea; emotional lability; flatulence; gait abnormal; gastrointestinal discomfort; headache; hypertension; increased risk of infection; insomnia; leucopenia; malaise; movement disorders; muscle complaints; nausea; nystagmus; oedema; pain; reflexes abnormal; seizure (in children); sensation abnormal; sexual dysfunction; skin reactions; thinking abnormal; tooth disorder; tremor; vasodilation; vertigo; visual impairment; vomiting
Pregabalin (Lyrica)
Description: Antiepileptic Dose: Initially 150 mg daily in 2–3 divided doses, then increased if necessary to 300 mg daily in 2–3 divided doses, dose to be increased after 3–7 days, then increased if necessary up to 600 mg daily in 2–3 divided doses, dose to be increased after 7 days.
Common side effects: Abdominal distension; appetite abnormal; asthenia; cervical spasm; concentration impaired; confusion; constipation; diarrhoea; dizziness; drowsiness;dry mouth; feeling abnormal; gait abnormal; gastrointestinal disorders; headache; increased risk of infection; joint disorders; memory loss; mood altered; movement disorders; muscle complaints; nausea; oedema; pain; sensation abnormal; sexual dysfunction; sleep disorders; speech impairment; vertigo; vision disorders; vomiting; weight changes
Amitriptyline ( Elavil)
Description: Anticholinergic Dose: Initially 10–25 mg daily, dose to be taken in the evening, then increased, if tolerated, in steps of 10–25 mg every 3–7 days in 1–2 divided doses; usual dose 25–75 mg daily, dose to be taken in the evening, doses above 100 mg should be used with caution (doses above 75 mg should be used with caution in the elderly and in patients with cardiovascular disease); maximum per dose 75 mg.
Common side effects: Anticholinergic syndrome; (agitated (hyperactive) delirium – typically including confusion, restlessness and picking at imaginary objects) drowsiness; QT interval prolongation ( heart rhythm)
Caution in: chronic constipation, urinary retention
Frequency not known includes: visual disorders, confusion, constipation, dizziness, impaired concentration, peripheral neuropathy, urinary retention, altered sensation and depression, all of which can be confused with symptoms of MS; anticholinergics are also associated with dementia in long term use ( over 2 years)
Duloxetine ( Cymbalta)
Description: serotonin and noradrenaline re-uptake inhibitors (SNRI)
Dose: Initially 30 mg once daily, increased if necessary to 60 mg once daily; maximum 120 mg per day.
Common side effects: Anxiety; appetite decreased; constipation; diarrhoea; dizziness; drowsiness; dry mouth; fall; fatigue; flushing; gastrointestinal discomfort; gastrointestinal disorders; headache; muscle complaints; nausea; pain; palpitations; paraesthesia; sexual dysfunction; skin reactions; sleep disorders; sweat changes; tinnitus; tremor; urinary disorders; vision disorders; vomiting; weight changes; yawning
Capsaicin cream ( Axsain)
Description: plant alkaloids Dose: Apply 3–4 times a day for 8 weeks then review, dose to be applied sparingly, not more often than every 4 hours.
Common side effects: abnormal sensation.
Caution: avoid contact with eyes; avoid hot shower or bath just before or after application (burning sensation enhanced); avoid inhalation of vapours; not to be used under tight bandages
Tramadol (Zydol)
Description: Opioid Dose: For use as short term ‘rescue therapy ‘ only
Initially 50 mg, then, adjusted according to response; Usual maximum 400 mg/24 hours, or use modified release over 12 or 24 hours preparations
Common side effects: Arrhythmias; confusion; constipation; dizziness; drowsiness; dry mouth; euphoric mood; flushing; hallucination; headache; hyperhidrosis; hypotension (with high doses); miosis; nausea (more common on initiation); palpitations; respiratory depression (with high doses); skin reactions; urinary retention; vertigo; visual impairment; vomiting (more common on initiation); withdrawal syndrome
Secondline medications
Medication & Example brand name
Description, Dose, Side effects
Only the most common side effects are listed; before recommendation or prescription, read full list of possible side effects at https://bnf.nice.org.uk/
High strength capsaicin patch (Qutenza)
Description: plant class alkaloids Dose 179mg patch
Common Side effects: sensation abnormal
Cautions: avoid contact with the face, scalp or in proximity to mucous membranes; avoid holding near eyes or mucous membranes; recent cardiovascular events; uncontrolled hypertension
Lidocaine patch (Versatis)
Description: local anaethetic Dose: Apply once daily for up to 12 hours, followed by a 12-hour plaster-free period; discontinue if no response after 4 weeks, to be applied to intact, dry, non-hairy, non-irritated skin, up to 3 plasters may be used to cover large areas; plasters may be cut.
Common side effects in intravenous use – as systemic absorption can follow topical administration, should be borne in mind:
anxiety; arrhythmias; atrioventricular block; cardiac arrest; circulatory collapse; confusion; dizziness; drowsiness; euphoric mood; headache; hypotension (may lead to cardiac arrest); loss of consciousness; methaemoglobinaemia; muscle twitching; myocardial contractility decreased; nausea; neurological effects; nystagmus; pain; psychosis; respiratory disorders; seizure; sensation abnormal; temperature sensation altered; tinnitus; tremor; vision blurred; vomiting
Venlafaxine (Effexor)
Description: SNRI Dose: initially 75 mg daily in 2 divided doses, then increased if necessary up to 375 mg daily, dose to be increased if necessary at intervals of at least 2 weeks, faster dose titration may be necessary in some patients; maximum 375 mg per day. Common Side effects: Anxiety; appetite decreased; arrhythmias; asthenia; chills; confusion; constipation; depersonalisation; diarrhoea; dizziness; dry mouth; dyspnoea; headache; hot flush; hypertension; menstrual cycle irregularities; movement disorders; muscle tone increased; mydriasis; nausea; palpitations; paraesthesia; sedation; sexual dysfunction; skin reactions; sleep disorders; sweat changes; taste altered; tinnitus; tremor; urinary disorders; vision disorders; vomiting; weight changes; yawning
Tapentadol (Palexia, Nucynta)
Description: Opioid with SNRI: Dose: Modified release:Initially 50 mg every 12 hours, adjusted according to response; maximum 500 mg per day Side effects: Anxiety; appetite decreased; asthenia; diarrhoea; feeling of body temperature change; gastrointestinal discomfort; muscle spasms; sleep disorders; tremor; for all opioids: Arrhythmias; confusion; constipation; dizziness; drowsiness; dry mouth; euphoric mood; flushing; hallucination; headache; hyperhidrosis; hypotension (with high doses); miosis; nausea (more common on initiation); palpitations; respiratory depression (with high doses); skin reactions; urinary retention; vertigo; visual impairment; vomiting (more common on initiation); withdrawal syndrome
A non – opioid medication that can sometimes help persistent pain which does not respond to other medications, is Nefopam hydrochloride. Possible side effects include nausea, dizziness, lightheaded, nervousness, confusion, dry mouth, urinary retention.
Other medications that may be offered include stronger opioids, eg morphine, oxycodone, buprenorphine. See using opioids for more information.
NHS guidelines state that these should only be prescribed in specialist centres, such as a pain clinic or neurology clinic. This is not necessarily because they are stronger, but generally because they are not licensed for the treatment of pain, but for other uses, and have less evidence for use in pain.
Secondline medications for neuropathic pain that can be prescribed via specialist clinic include, but are not limited to:
For pain that does not respond to standard treatment, ask to be referred to a pain clinic. These vary greatly around the country in terms of what they offer, but may offer acupuncture, psychological therapies, electrotherapies as well as medications and injections.
Pain clinics, also offer various types of injections for different pains, the ones most likely to be suitable in MS are
- Nerve block injections for neuralgias
Thirdline interventions
- Intravenous lidocaine (relief only tended to last for up to 28 days)
- Intravenous ketamine
The evidence for these two treatments is not robust, and there are only a few centres that offer them, but I have met people for whom it has been the only thing that has helped them.
- Deep Brain Stimulation. This invasive procedure involves stimulating a precise area of the brain using an electrode to modulate the central processing of pain signals.
This procedure is carried out on the NHS, but as there are serious and well-known risks, it is reserved for the most difficult pain conditions.
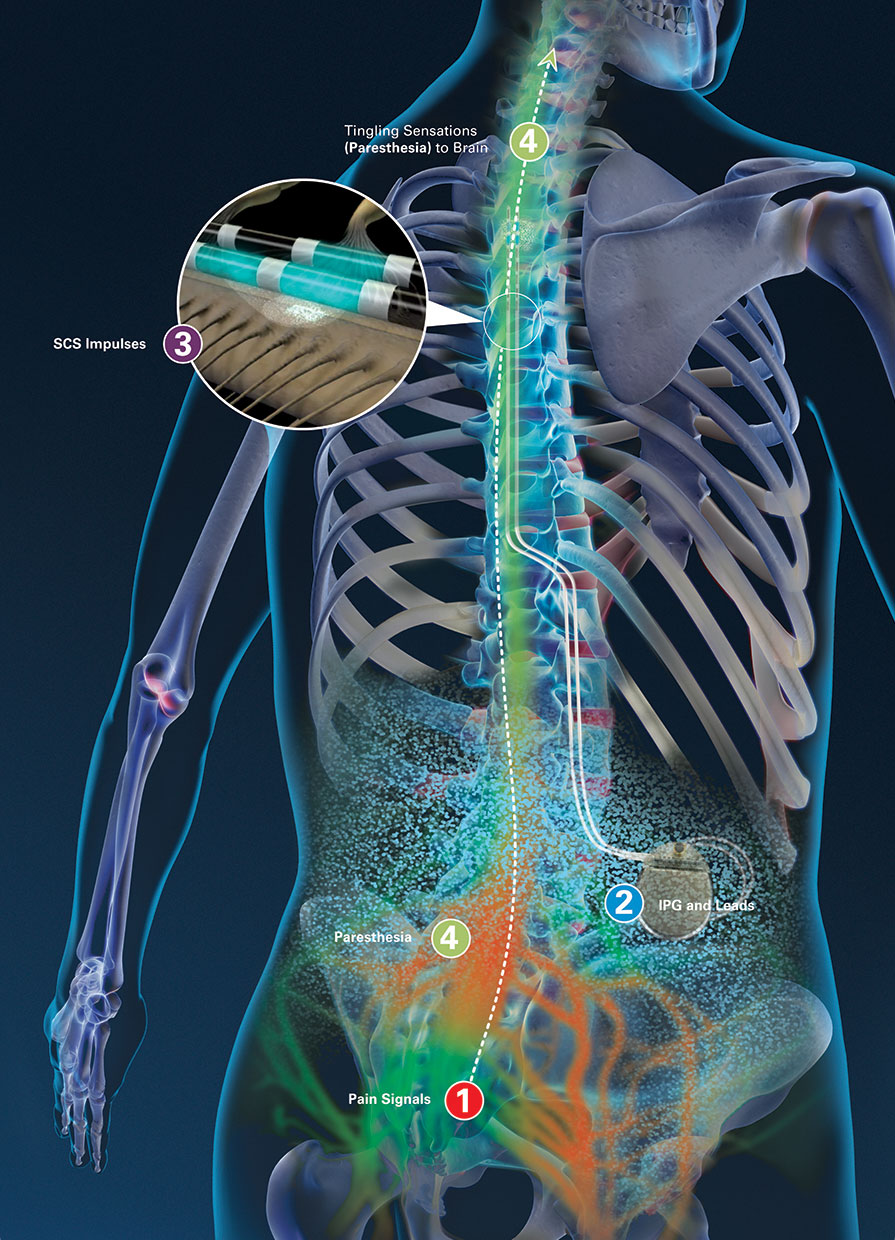
- Spinal cord stimulation (SCS) SCS is an invasive procedure where a small electrical stimulator is placed on the spinal cord, to modify the perception of neuropathic and ischaemic pain.
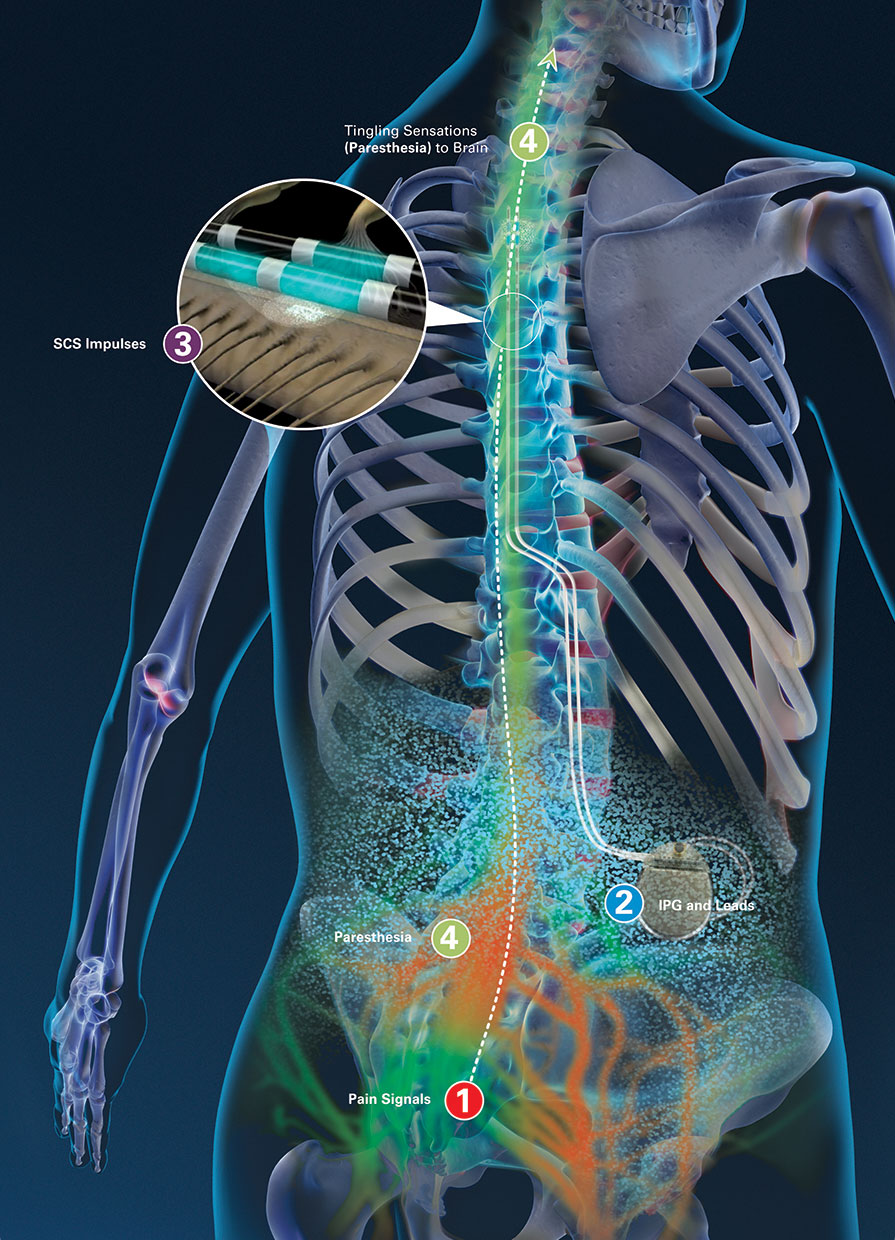
picture: Boston Scientific
SCS is also available as a treatment for chronic neuropathic pain, both on the NHS and privately, but as it has a cost of around £10,000 per patient and a life of around 3-4 years, it is usually considered after standard treatments have failed. It works in the same way as a TENS machine, so ‘accommodation’, or the body becoming used to the current and needing a stronger stimulus, can be a problem over time.
Implanting of devices to relieve pain is known as neuromodulation, and techniques are evolving. Newer techniques include Dorsal root ganglion stimulation, dorsal root ganglion paddle stimulation, and high frequency spinal stimulation.
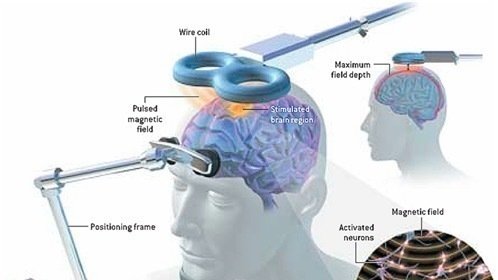
- Transcranial Magnetic Stimulation (TMS)
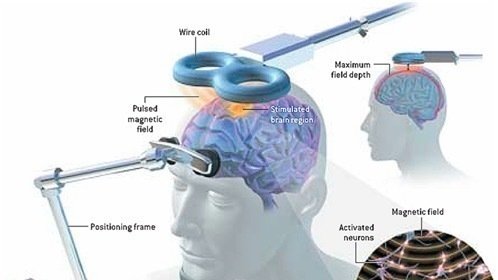
Also known as repetitive, or rTMS, is a new, non-invasive treatment that involves having a magnetic pulse sent to the brain from a plastic-coated magnetic coil held against the head. At present it has only been licensed o the NHS for treatment of depression, but there is also evidence for its use in neuropathic pain. At present it is only available for pain on the NHS as part of research at one centre in the UK; the Walton centre in Liverpool
- Transcranial direct current stimulation ( tDCS)
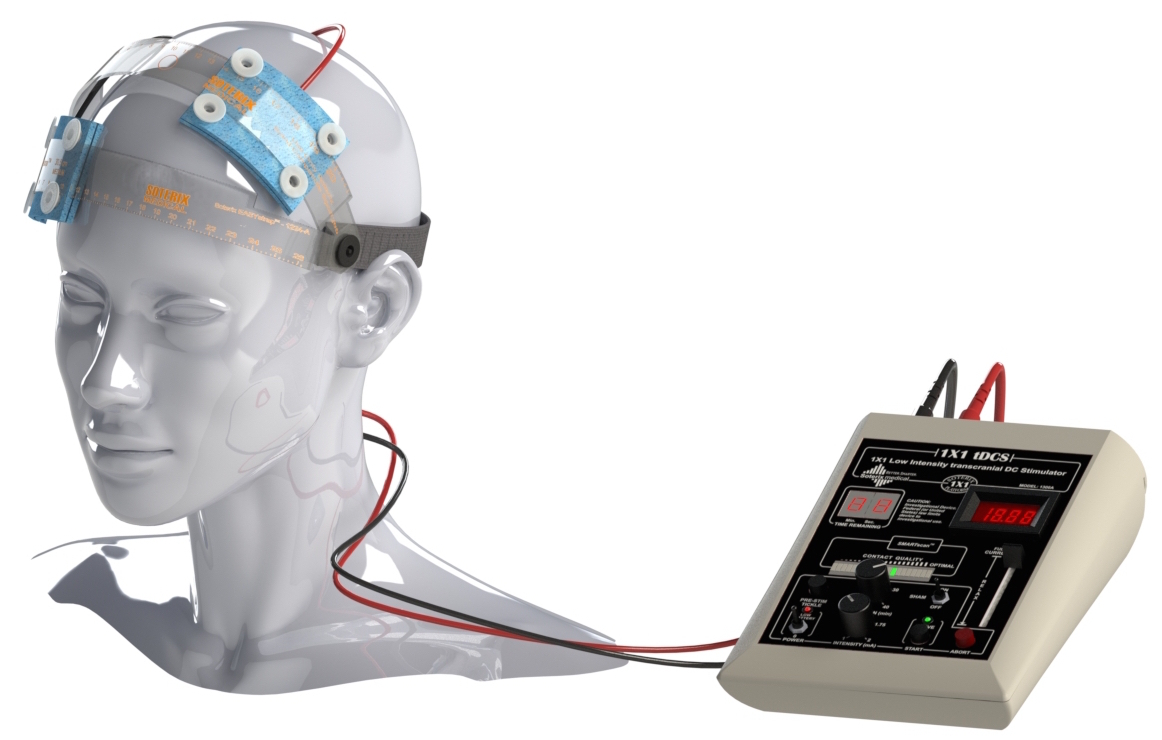 tDCS is a non-invasive method of electrical stimulation of the brain using a weak direct current applied to the scalp through electrodes, using a portable, battery operated device. At present it is only available on the NHS for treatment of depression. However, there has been one study in 19 people with MS, which found a 37% decrease in pain over around 4 weeks. tDCS is available privately, and hand held devices are available for purchase. People have been excitedly using privately bought units to make themselves smarter, more alert, or game faster, but there is a possiblity that units could be used for pain control.
tDCS is a non-invasive method of electrical stimulation of the brain using a weak direct current applied to the scalp through electrodes, using a portable, battery operated device. At present it is only available on the NHS for treatment of depression. However, there has been one study in 19 people with MS, which found a 37% decrease in pain over around 4 weeks. tDCS is available privately, and hand held devices are available for purchase. People have been excitedly using privately bought units to make themselves smarter, more alert, or game faster, but there is a possiblity that units could be used for pain control.
Safe non-pharmaceutical options for home use
Some people find that cooling strategies give temporary relief, including wearing ‘freezer socks’ ( socks that have been put in the freezer!) cooling garments, and cooling gels
For allodynia, (pain from something that does not normally cause pain, such as shoes, clothing or bedclothes touching the skin) wearing things that provide a continuous stimulus, such as gloves, tight lycra clothing, or lycra splinting /dynamic movement orthoses may help. A bed cradle can be used to keep duvet/bedclothes off the feet, and sheepskin booties can relieve the weight of feet rubbing on the mattress.

dynamic movement orthoses
Electrotherapies are the only non-pharmaceutical options with published evidence of effectiveness in neuropathic MS pain. There is ‘very low quality’ evidence (small studies, lack of comparative data) for use of TENS in neuropathic pain in MS, and this definitely helps some people. A TENS device can be worn for long periods, with the unit clipped to a belt. There is as yet unpublished data on a micro-current electrotherapy, Action Potential Simulation, or APS Therapy. We have had a lot of success with this in the MS Therapy centre where I work, and it is now offered by 11 other MS centres around the UK, or can be used at home.
Although evidence is limited due to the lack of randomised controlled trials, there are many other mind-body therapies that are used by people with MS; the two that have been studied in most detail are acupuncture and mindfulness. See complementary therapies, and ‘For all types of persistent pain’
Controversial / less safe / possibly pharmaceutical
Cannabis and cannabinoids
Cannabis is a naturally occurring drug made from parts of the cannabis plant. It contains many different compounds which are known as cannabinoids, the most widely studies are THC ( the part that makes people ‘high’) and CBD.
In the UK, cannabis is a controlled drug, Class B under the Misuse of Drugs Act 1971, and currently assigned to Schedule 1, so it cannot be prescribed or held legally with a prescription. Changes to the law are expected, see https://www.mstrust.org.uk/news/views-and-comments/medicinal-cannabis-%E2%80%93-a-potted-guide
In the meantime, many people with MS do find cannabis useful, and use it in various ways, including growing it, making tinctures, vapes, and using it in foodstuffs. There are certain risks to mental and physical health, specifically for those who are younger than 25 years of age, might be pregnant, have cardiovascular disease, respiratory disease, a history of psychosis, or a substance use disorder.
Cannabinoid medication: Sativex is an under the tongue spray, which contains both THC and CBD and has been licensed for spasticity in the UK, but not pain. This information, updated November 2019, is from the MS Trust:
Sativex is a licensed treatment and can be prescribed legally in the UK, but NHS prescribing remains limited and varies across the country.
In England, NICE guidance recommends that, providing the local NHS health authority is willing to pay for continued treatment, a 4-week trial of Sativex can be offered to people with moderate to severe MS-related spasticity which has not improved while taking other treatments. At the end of the trial, if their spasticity-related symptoms have improved by at least 20%, they can continue taking Sativex.
In Wales, it can be prescribed for moderate to severe spasticity in people with MS who haven’t responded to other anti-spasticity medication.
In Scotland and Northern Ireland, Sativex is currently not considered a cost effective treatment.
Limited access to Sativex on the NHS means that some people decide to obtain a private prescription and pay for the cost of the drug themselves. This can be an expensive option and it’s therefore not feasible for everyone.
It can only be prescribed by a specialist doctor with experience of treating MS spasticity – consultant neurologists, consultant rehabilitation specialists and consultant pain specialists.
Use of Sativex is currently limited to those people who respond to the first four weeks of treatment. If there is no clear improvement in spasticity-related symptoms, treatment is stopped.
 CBD oil, which is available from health food stores and online retailers, is made from cannabis but has had the THC removed. In research, only cannabis preparations with a high level of THC have been found to be effective for neuropathic pain in MS in clinical trials. However, people’s anecdotal experience suggests that for some, good quality/high strength CBD oil preparations can be helpful; possibly because for some it relaxes, reducing anxiety and making people feel more distanced from the pain.
CBD oil, which is available from health food stores and online retailers, is made from cannabis but has had the THC removed. In research, only cannabis preparations with a high level of THC have been found to be effective for neuropathic pain in MS in clinical trials. However, people’s anecdotal experience suggests that for some, good quality/high strength CBD oil preparations can be helpful; possibly because for some it relaxes, reducing anxiety and making people feel more distanced from the pain.
There is a thoughtful post about this on the chronic pain blog site, Healthskills, here:
People sourcing CBD oil should be aware of possible interactions with other drugs.
For all types of persistent pain
Modulating pain
Pain is a sensory and emotional experience, not always related to damage in any physical structure. It occurs in the brain, and not in the part of the body that hurts.
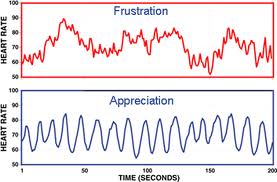
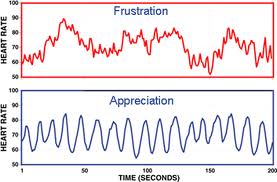
All pain can be ‘modulated’ – turned up or turned down, at different places along the path of the nerve, and emotions have been found to affect how strong the pain feels at different times. Your brain is only able to cope with a certain amount of information at one time, and this includes pain.
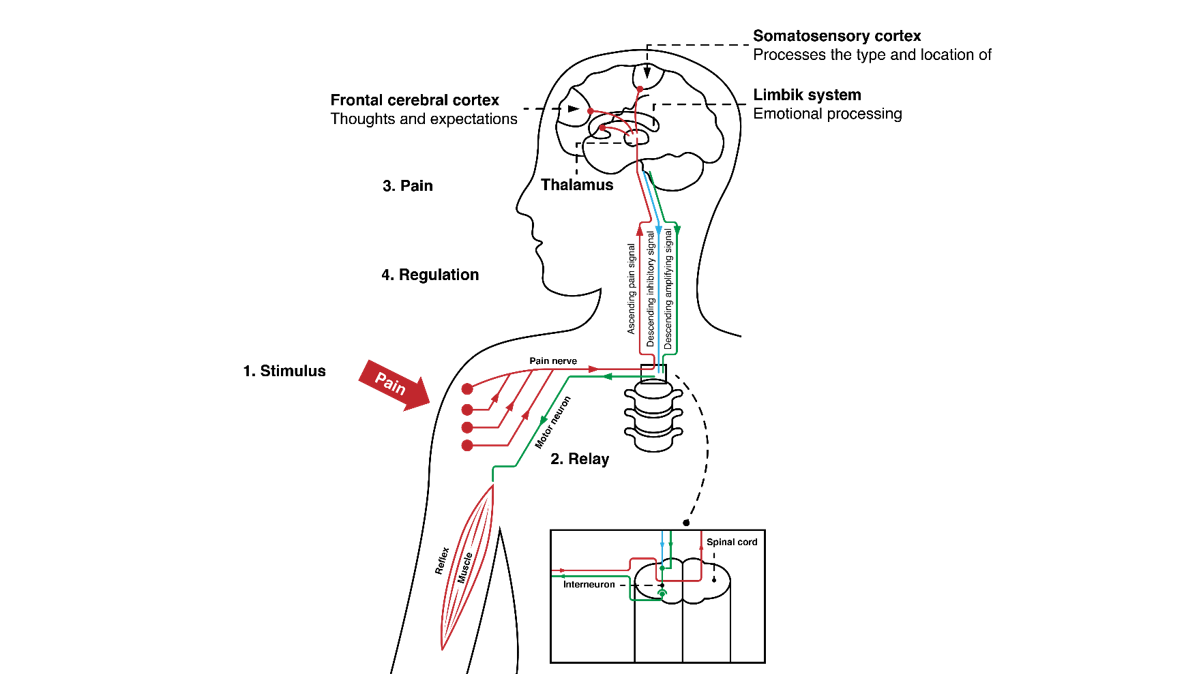 Factors that ‘wind up’ or heighten the pain response include ;
Factors that ‘wind up’ or heighten the pain response include ;
Hyper-vigilance – focussing on the pain
Fear
Anxiety
Stress
Previous negative experience
Beliefs about meaning of pain
Criticism – being criticised!
Boredom
Depression
Factors that ‘wind down’ or de-escalate the pain response include:

○ Relaxation
○ Distraction, enjoyment
○ Meditation/ Mindfulness
○ Meaning
○ Social bonding/ interaction
In chronic / persistent pain, the pain is no longer a warning about damage, and as such does not serve any useful purpose. In many types of persistent pain, the most useful approach is to focus on living a fulfilling life with pain, without giving up on seeking out things that help.
Free Resources
The best free resource that I have found to learn about managing chronic/persistent pain is ‘Retrain Pain’ at https://www.retrainpain.org/
The Pain Toolkit can also be useful, but it’s more geared towards musculoskeletal pain:
These blogs contain a lot of insight about living with persistent pain; the first aimed at people with pain

and the second for healthcare professionals
It may also possible to be referred to locally taught pain management / supportive courses such as:
- Self management programmes (SMPs)
- NHS pain management programmes (PMPs)
And for exercise, ‘Exercise on referral/prescription’ courses at a local gym.
You can also access online NHS exercise studio videos at https://www.nhs.uk/conditions/nhs-fitness-studio/
Privately bought pain management resources include
- Book and CD set: Mindfulness for Health: A practical guide to relieving pain, reducing stress and restoring wellbeing, by Danny Penman
- The ‘Headspace’ app pain management pack is introduced here:
https://www.headspace.com/blog/2017/03/31/headspace-for-pain-management/
and the day 1 meditation is here: https://my.headspace.com/packs/36
- I have always found HeartMath biofeedback to be the most effective system for creating resilience to stress, and use in in my MS clinic, where I did a small piece of research some years ago. There are also some published studies showing reduction in chronic pain when using this system. This is a simple technique that can be taught using biofeedback software by a licensed trainer, or used with a privately bought app and biofeedback sensor.


I hope that by reading through this you will find something that helps on your journey with pain.
-Please let me know about anything that you think I’ve missed out; or mistakes – the topic is so vast! Also your experiences with things that do help you, so that I can continue to increase my knowledge and understanding, and pass on useful information to the people that I see, both in my MS Nursing clinic, and in my business life with Action Potential Simulation therapy.
Thanks, and
All the very best!
Miranda











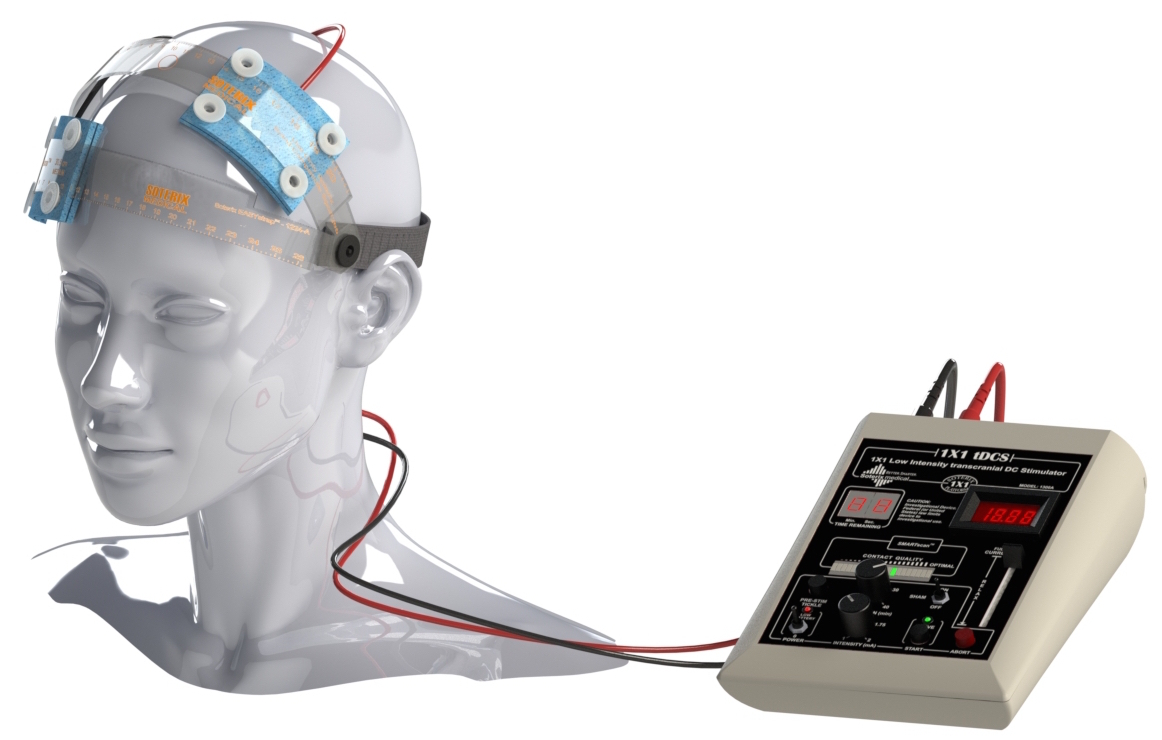 tDCS is a non-invasive method of electrical stimulation of the brain using a weak direct current applied to the scalp through electrodes, using a portable, battery operated device. At present it is only available on the NHS for treatment of depression. However, there has been one study in 19 people with MS, which found a 37% decrease in pain over around 4 weeks. tDCS is available privately, and hand held devices are available for purchase. People have been excitedly using privately bought units to make themselves smarter, more alert, or game faster, but there is a possiblity that units could be used for pain control.
tDCS is a non-invasive method of electrical stimulation of the brain using a weak direct current applied to the scalp through electrodes, using a portable, battery operated device. At present it is only available on the NHS for treatment of depression. However, there has been one study in 19 people with MS, which found a 37% decrease in pain over around 4 weeks. tDCS is available privately, and hand held devices are available for purchase. People have been excitedly using privately bought units to make themselves smarter, more alert, or game faster, but there is a possiblity that units could be used for pain control.

 CBD oil, which is available from health food stores and online retailers, is made from
CBD oil, which is available from health food stores and online retailers, is made from 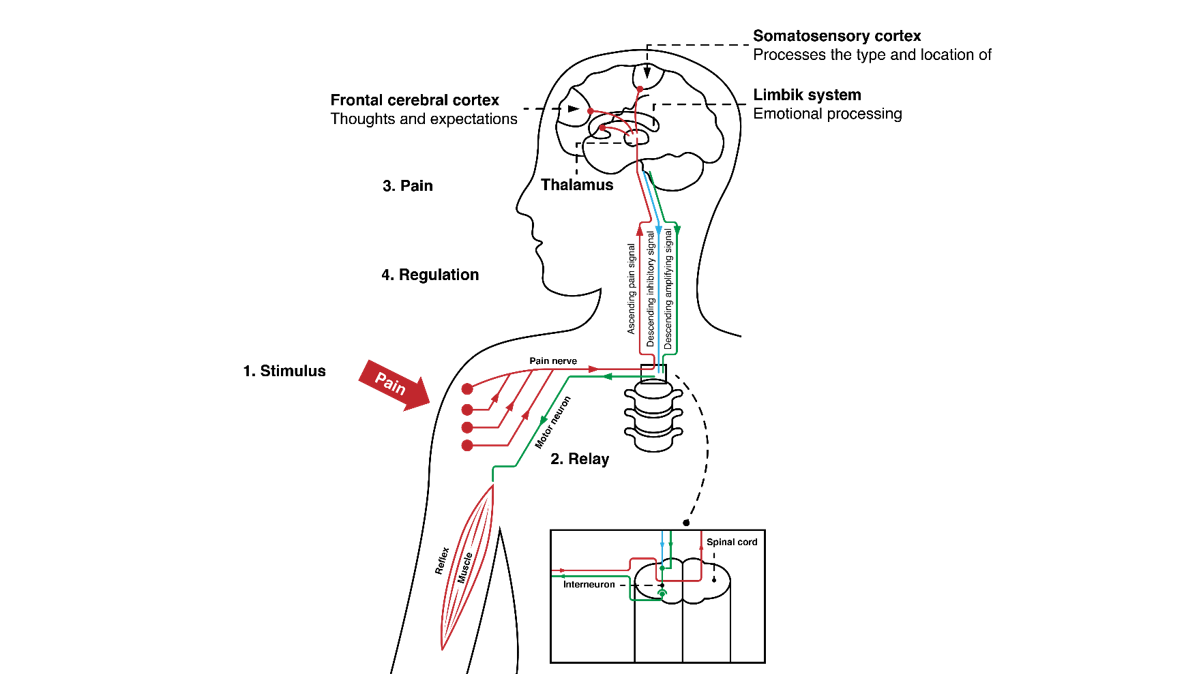 Factors that ‘wind up’ or heighten the pain response include ;
Factors that ‘wind up’ or heighten the pain response include ;























 Amitriptyline, Carbamazepine, Gabapentin, Pregabalin, and Baclofen as well as opiod painkillers, antidepressants, blood pressure drugs, statins, and cannabis.
Amitriptyline, Carbamazepine, Gabapentin, Pregabalin, and Baclofen as well as opiod painkillers, antidepressants, blood pressure drugs, statins, and cannabis.
 than a sex toy, whose aim is to improve blood flow to the clitoris, using a little suction cup device, making orgasm more likely! In a study of (only 15) women diagnosed with sexual dysfunction, more than 80% reported increased sexual satisfaction, and 55% achieved orgasm; they also reported more genital sensation and vaginal lubrication, when using Eros.
than a sex toy, whose aim is to improve blood flow to the clitoris, using a little suction cup device, making orgasm more likely! In a study of (only 15) women diagnosed with sexual dysfunction, more than 80% reported increased sexual satisfaction, and 55% achieved orgasm; they also reported more genital sensation and vaginal lubrication, when using Eros.














