Action Potential Simulation Therapy ( APS Therapy) for pain in people with MS; Report on a One Year Pilot Study.
Miranda Olding RGN MSCN, Denise Kehoe
Abstract
People with MS commonly suffer from both nociceptive and neuropathic pain, and the latter is often resistant to treatment, or hard to resolve due to the unwanted side-effects of most of the appropriate drugs.
We carried out a one year pilot using the electrotherapy device APS Therapy to treat pain in people with MS, at the voluntary sector multi-disciplinary MS Therapy Centre, in Bedford, UK.
An 8 week course of the therapy 3 times a week was offered initially, and 38 people used APS Therapy to treat 61 different pains.
Within 8 week periods, 28 people (76%) got beneficial reduction in pain. Of the 58 pains, 50 (86%) had a reduction of at least one point on the Visual analogue Scale (VAS) for pain. Of the pains that improved, 17 (30%) were reduced to pain free. The average reduction in points on the VAS was 4.7 points. 12 people reduced or discontinued medications as a direct result of the effects of APS Therapy; with more structured review and supervision, we feel that this number could be higher, and have adjusted our practice accordingly.
Many participants reported improved sleep and enhanced energy, and the improved quality of life that this afforded.
Many of the participants who benefitted, especially those with chronic neuropathic pain, felt that they needed long term treatment, but were able to maintain the benefits sustained at a reduced frequency of treatment ( once a week or even fortnightly), and elected to carry on. We were able to offer this as an ongoing service.
Robust research on APS Therapy is scant, but based on the outstanding results of this pilot is a very promising area for further research and clinical treatment.
Introduction
The problem of pain in the UK
Pain is defined as ‘An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ (1)
Chronic pain is defined as continuous, long-term pain of more than 12 weeks or after the time that healing would have been thought to have occurred in pain after trauma or surgery.( 2)
Almost eight million people in the UK have chronic pain, or an estimated one in 5 Europeans. (3) As well as the human suffering, it also represents a significant burden to wider society and economies. Chronic pain accounts for 4.6 million GP appointments every year at a cost of £69 million. Expenditure is on referrals, appointments, prescribing, consequences of ineffective home prescribing and adverse events. (4)
Current medical treatment centres around medication, but drug treatments often cause unwanted side effects or other medical problems, and the costs of drugs for managing pain alone in England in 2009 amounted to £449 million. (5)
Access to pain management services in the UK is inconsistent and available health services for pain differ markedly in the type of care they offer.(6)
Although in some chronic pain clinics, TENs, acupuncture, physical, psychological techniques, invasive treatments, and complementary therapies are offered, availability varies widely, rates of successful pain resolution are low, and 38% of people with chronic pain report inadequate pain management.(7,8, 9)
The problem of pain in MS
Estimates vary as to the proportion of people with MS who suffer from pain, with some reports suggesting that up to 80% of people with MS may suffer from pain at some stage. (10,11,12)
People with MS commonly suffer from both types of pain; both nociceptive (‘normal’ type, after injury or with inflammation) and neuropathic. Neuropathic pain is defined as ‘pain caused by a lesion or disease of the somatosensory nervous system’ (13) is often characterized as burning, severe shooting pains, and/or painful numbness or tingling. It is commonly a long term or chronic pain, and effective treatment is difficult as the classes of drugs to which it responds best are associated with various adverse effects. ( sedation and weight gain most commonly) (14)
The aim of treatment is to minimise the level of pain and to develop coping strategies so that the individual can carry out normal day-to-day living. Treatment options include drugs and non-drug treatments such as physiotherapy, electrotherapy or a combination.
Electrical therapies
There are many modalities of electrical therapies currently in use within physical therapy for pain relief and injury repair, which have been categorised into 3 broad areas(15)
Electrical stimulation agents, including Transcutaneous Electrical Nerve stimulation (TENS), Action Potential Simulation Therapy (APS Therapy), Interferential Therapy (IFT), Functional Electrical Stimulation (FES), and Microcurrent therapy (MCT),
Thermal modalities, including Infra red Irradiation (IFR), Therapeutic Ultrasound and Laser Therapy, and
Non Thermal Modalities including Pulsed Ultrasound, Pulsed Electromagnetic Fields (PEMFs) and Microcurrent Therapy (MCT)
The most commonly used form of electrotherapy in healthcare is TENS. This uses an alternating current to affect pain gate mechanisms. A Cochrane review concludes that ‘despite the widespread use of TENS machines, the analgesic effectiveness of TENS still remains uncertain’(16)
There are many studies demonstrating its’ usefulness, however, in my experience with MS it has only occasionally been effective for mild or moderate pain, but has been limited to the duration of treatment with the electrodes, or a one or two hour carryover at best.
We heard about some exceptional case studies carried out in Hull using the electro-therapy Action Potential Stimulation (APS)Therapy showing effectiveness in reducing both pain and fatigue; drastically reducing the medication used, and increasing mobility, independence and quality of life in people with MS(17) and decided to investigate.
APS Therapy
APS Therapy ( Action potential simulation therapy) is a type of micro-current therapy.
These therapies involves application of electric currents of similar form and magnitude to those produced naturally by the body and there is evidence that this can promote healing in a variety of damaged tissues. (18)
The APS Therapy device uses an electrical current that supposedly mimics the normal physiological action potential of nerve conduction. The device is said to produce action potentials that are four times stronger than those naturally occurring in the neuron. When swelling, inflammation, poor circulation and pain occur due to mechanical, chemical or electrical disturbances, by stimulating the body’s natural regenerative processes (as in depolarisation), it is postulated that these conditions are encouraged to resolve. (19) See discussion.
Literature review for micro-current and APS Therapy
A literature review on over 70 papers on micro-current therapy in 2009 concluded that there was evidence for its use with non-uniting fractures, spinal fusions and a skin ulcers, particularly where other forms of treatment had not been successful; that In vitro studies also suggest that there is unexplored potential for its use in musculoskeletal disorders. However, higher quality and more comprehensive research is needed. (20)
An assessment of APS Therapy on 285 Patients with Chronic Pain in 2002 reported a mean average VAPS was 6.8 before treatment and 3.3 after treatment in the over 50s, and 6.3 and 2.2 respectively in the under 50s. Out of the 285 patients,44 (15%) ended with a ‘0’ VAPS and 199 (69%) with a score of 5 or less. (21)
A trial of APS Therapy in patients awaiting or having neurosurgery for intractable spinal pain concluded that the number of patients treated was too low to reach a statistical conclusion, but that the trend was very promising and they recommended that patients waiting for destructive surgery should first be put on a thorough trial of APS Therapy.(22)
In a 1999 randomized, patient blinded, placebo-controlled study, on 76 patients with chronic osteoporotic back pain, reported pretreatment baseline VAPS value average of of 57.79, and post- treatment value after the sixth treatment of 9.7 (p= 0,0001); 6 patients maintained benefits 6 months post treatment.(23)
A study in 1999 on APS Therapy compared with TENS in 99 patients with osteoarthritis of the knee did not find a significant difference between the two treatment groups given just 6 treatments over a 2 week period. The authors did note, however, that the APS group showed a significant improvement in measures of knee flexion and swelling, which persisted even 1 month after the last treatment. (24)
Methods
Sample
People with MS who presented with pain in the MS Nurse’s clinic were screened for suitability and contra-indications, and offered the chance to trial the therapy. Pain due to spasticity/muscle spasm , or pain whose origin was uncertain, where more investigations were needed, were excluded.
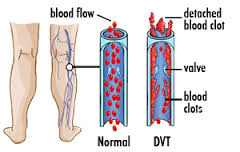
Contra-indications include having a Pacemaker, epilepsy, pregnancy, or cancer, or in the past 3 months, stroke, heart attack, deep vein thrombosis or pulmonary embolus. One participant had a baclofen pump; after discussion with the manufacturers of both devices, this was allowed in this case. We also checked that participants felt able to drink the recommended litre and a half of water daily during therapy.
All the participants gave their informed consent to take part in the study; it was made clear that this was optional. 39 had MS, 3 did not. ( 2 were members of staff, and one a volunteer)
An 8 week course of APS Therapy, with 3 x sessions a week, comprising of 4, back to back 8 minute electrode placements, was offered, in a clinic room at the multi-disciplinary, voluntary sector MS Therapy Centre in Bedford, UK. We had first one, and then 2 APS Therapy clinic machines. People who could apply the electrodes themselves had one teaching session and then self-treated, with floating supervision from staff.
During the 8 week course, 6 people dropped out. One had vomiting and headache after 1st treatment, decided not to proceed. Detoxification reactions ( usually headache) are possible, although not common if drinking the recommended amount of water, and are self-limiting. One experienced flickering in her vision and decided not to proceed. Although there is no documented precendent for this, and the cause was uncertain, electrotherapies can trigger migraine in susceptible people. Three people became unwell, two with existing other conditions and one with an MS relapse since starting treatment and either unable or decided not to proceed. One struggled to travel for treatment and felt discouraged after no benefit felt at 2& ½ weeks.
36 people in this study went on to use APS Therapy to treat 58 different pains.
25 of the pains were neuropathic, including 2 sciatic type pains, and 34 were nociceptive, including headaches, fibromyalgia type tender spots, backache, joint pain and arthritic type pain.
32 were women and 4 were men. The average age was 52 for women and 51 for men. 11 people had relapsing remitting MS, 22 had primary or secondary progressive, and 3 did not have MS.
We measured pain using the visual analogue pain scale (VAS), asking each participant to score for the average, or constant level of pain, and the worst level of pain, and how much of the time the pain was average, how much of the time worse. Medication use was recorded.
Results:
In 8 week periods;
Of the 36 people, 28 (78%) had reduction in pain.
Of the 58 pains, 50 (86%) had reduction.
Of the pains that improved, 17 pains (30%) went down to 0/10, or pain free.



Reduction’ was quantified as 1 or more whole points on the VAS for pain. Neuropathic pains appeared to respond almost as well as nociceptive pains to the treatment12 people reduced or discontinued medication as a direct result of the results of the APS Therapy, on reflection, with more supervision, we feel that this could have been more.The mean pre-treatment score on the VAS for ‘Average level of pain’ overall was 5.56. Mean reduction in pain was 4.7 points, to a mean post-treatment VAS of 2.3.Average reduction for ‘worst pain’ scores was 4.1 points on the VAS scale.

Neuropathic pain
nb. in the charts below, a score of 0 or pain free, has been represented by a score of 0.01, in order to show up as a colour.

‘Average pain’ in the 14 cases of neuropathic feet and legs had a mean pre-treatment score of 6.3, which reduced by 3.8 points on the VAS on average to 2.5.
2 individual’s pain did not respond at all, 12 people experienced a benefit, and of these, 5 people went to pain free.

‘Worst pain’ for neuropathic feet and legs was a pre treatment mean of 8.03, and reduced by 5.17 on the VAS on average, to a post treatment mean of 2.46, with 5 people at pain-free.
Combined ‘average’ and ‘worst’ pain scores gave a mean reduction of 4.5 points on the VAS.
Other neuropathic or nerve pain:
In neuropathic pain of the trunk, arms, hands and face, reduction in ‘average pain’ was a mean of less, at 2.5, but still had a reduction in ‘worst pain’ of 4.9 points on the VAS.


Joint pain or injury
‘Average pain’ scores for joint pain or injury had a pre treatment mean of 5.1 and fell 2.9 points on the VAS to a mean of 2.2 . Actual results were quite polarised, with 4 people having no response, and 7 going to pain free.

‘Worst pain’ for the 16 joint type pains had a pre treatment mean of 7.5 points on the VAS, and fell by an average 4.9 points on the VAS to a mean of 2.6. 2 people’s worst pain did not respond, and 7 pains went to pain free.

Headaches
People with headaches responded particularly well to APS Therapy; the reduction in ‘average pain’ as scored by the VAS was 4.7, but our data does not catch the reduced incidence in those still experiencing headaches.

Back pain
‘Average pain’ for back pain had a response of 3.3 points reduction on the VAS on average; 2 people’s pain got worse, one was unchanged, 7 benefitted, and of these, 2 went to pain free.

Other pains
The remaining pains were 2 cases of muscle fatigue type pain and one pain from metalwork post pin and plate, which did not respond, and 1 psoriasis pain and 1 varicose vein pain, both of which did benefit.

‘Other benefits’
For this report, we have not managed to keep accurate data about other benefits reported during APS Therapy treatment. These have been: 4 cases of significant improvement in energy/reduction in MS fatigue, 2 cases of significant reduction swollen legs and ankles, 1 report of improvement in skin discolouration due to poor circulation, reduction in size of ‘fatty lump’ on hip, swollen gland in neck, and fluid under the skin on the scalp, 2 cases of alleviation of life-long insomnia, and many reports of improvement in sleep quality. 2 people reported no further urinary tract infections, which had been recurrent, and which they attributed to the APS Therapy, and 1; reduction in dizziness and improvement in cognitive function, which again they attributed to the therapy, and reported as a post-treatment effect.
We have identified reliable and valid outcome measures that we will be using for future clinical governance to measure sleep quality and energy levels, and the effect of pain on everyday life and mood.
Discussion
One of our concerns when starting this project was that people might benefit, but need long term therapy, which we would not be able to offer long term. We hoped to be able to use the NHS one-off personal budgets to allow people to purchase their own machine if necessary, but the scheme was only available for people on continuing health funding in our area. In actual fact, we found that although we did have a group of people who needed to maintain therapy to maintain the benefit; but they were able to reduce the frequency of their treatment to once a week, or in one case once fortnightly, and still retain the effect, and a such we have been able to continue to provide a service for these people.
We did not have research funding for this study, there was no control group, and many variables. Our sample, as typical in MS, often had to cancel appointments due to health problems, transport or general difficulties, but still achieved a remarkable result.
It was interesting to note that effectiveness was similar between the neuropathic and nociceptive type pains when using APS Therapy.
The mode of action is not fully understood, but injury or disease can cause oedema, inflammation, neuronal dysfunction, circulatory disturbance and lack of oxygen supply to the tissues or organ systems. Inflammation in tissue also promotes the build-up of chemicals, known as the “inflammatory soup” which may interfere with neural transmission.
If there is poor transmission or even cessation of activity along the neurone, as a result of injury, inflammation, or disease process, the system cannot conduct its action potentials, and the homeostatic and regenerative mechanisms are disturbed.
It has been postulated by Papendorp (25) that introducing external action potentials through the use of APS Therapy may result in the metabolic catabolism and subsequent excretion from the body of inflammatory substances. As inflammatory metabolites may be a major cause of pain, removing the cause allows for pain reduction. Circulation is also improved and thus antibodies, enzymes, neurotransmitters and hormones are conveyed at an increased rate to the treated area, stimulating the body’s own healing mechanisms.
Conclusion
APS Therapy seemed to be a safe and effective therapy to try in cases of both neuropathic and nociceptive pain. Participants in this study, most of whom had MS, achieved positive results using APS Therapy in 76% of cases. The therapy was safe, and in the main, people were extremely happy with mode of treatment, preferring it to drug therapy, and in some cases reducing and discontinuing analgesic drugs as a result.
We hope that by presenting our pilot study of an APS Therapy service in the context of available research on the subject, we can stimulate further clinical use and research.
References
1) H. Merskey and N. Bogduk, Eds,.Classification of Chronic Pain, Second Edition, IASP Task Force on Taxonomy, IASP Press, Seattle, 1994.
2) British Pain society 2014 For media, FAQs http://www.britishpainsociety.org/media_faq.htm ( accessed 3/2/2014)
3) Breivik H, Collett B, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006 10( 4):pp 287-333
4) Belsey J. Primary care workload in the management of chronic pain: A retrospective cohort study using a GP database to identify resource implications for UK primary care. Journal of Medical Economics 2002 . 5, (1-4) pp 39-50
5) NHS Information Centre. Prescription Cost Analysis for England 2009. Available at: http://www.ic.nhs.uk
6) Harris M, Spence A, et al. (2000) Clinical Standards Advisory Group (CSAG): Services for patients with pain
7) Breaking through the Barrier’, Chief Medical Officer 2008 Annual Report, March 2000
8) InSites Consulting. Pain Proposal Patient and PCP Surveys. July – September 2010
9)Collett, B. Betteridge, N., Semmons, I , Trueman, P. Pain Proposal, Improving the current and future management of chronic pain 2010 http://www.arthritiscare.org.uk/…/main…/PainProposalUKSnapshotFinal.pdf
10) Ehde DM, et al.The scope and nature of pain in persons with multiple sclerosis. Multiple Sclerosis 2006;12(5):pp 629-638.
11) Hirsh AT, et al. Prevalence and impact of pain in multiple sclerosis: physical and psychologic contributors. Archives of Physical Medicine and Rehabilitation 2009;90(4):pp 646-651.
12) Archibald CJ, et al.Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients. Pain 1994;58(1):89-93.
13) International Association for the Study of Pain, 2011 http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Definitions (Accessed 3/2/2014)
14) Neuropathic pain – pharmacological management: the pharmacological management of neuropathic pain in adults in non-specialist settings. National Institute for Clinical Excellence November 2013
15) Watson, T. Narrative Review : Key concepts with electrophysical agents Physical Therapy Reviews 2010. 15(4): 351-359.
16) Cochrane Database Syst Rev. 2008 Jul 16;(3)
17) Van der Plaat, L. unpublished case studies using APS Therapy on people with MS in a day hospice setting. 2013
18) Berger P. Electrical pain modulation for the chronic pain patient. South African Journal of Anaesthesiologyand Analgesia. 1999;5:14-19.
19) Van Papendorp DH, Kruger MC, Maritz C, Dippenaar NG.
Medical Hypotheses- 2002 Elsevier
20) Watson, T. Narrative Review : Key concepts with electrophysical agents Physical Therapy Reviews 2010. 15(4): 351-359.
21) Papendorp DH van. (2002). Assessment of Pain Relief on 285 patients with chronic pain. Biomedical Research 2002; 26: 249-253.
22) Du Preez, J. Neurosurgical Pain Conditions University of Pretoria
23) Odendaal & Joubert APS Therapy- a new way of teating chronic backabacke, a pilot study South African Journal of Anaesthesiology and Analgesia.1999; 5 1
24) Berger, P. Matzner, L Study on 99 patients with osteoarthritis (OA) of the knee to investigate the effectiveness of low frequency electrical currents on mobility and pain: Action Potential Simulation therapy (APS) current compared with transcutaneous electrical nerve stimulation (TENS) and placebo.South Africa Journal of Anaesthesiology and Analgesia
1999 5: 2
25) ) Papendorp DH van. (2002). Assessment of Pain Relief on 285 patients with chronic pain. Biomedical Research 2002; 26: 249-253.
HOPE YOU LIKE IT!