Fatigue – that horrible overwhelming inability to do another thing, sometimes even to think straight, is one of the most disabling invisible problems of MS. When I took a poll of the top symptoms that people wanted to troubleshoot in a holistic way, Fatigue was top. So here goes:
 Why do people with MS experience fatigue?
Why do people with MS experience fatigue?
Fatigue in MS is of 2 types. Motor fatigue, or ‘short-circuiting’ fatigue, is when the difficulty of transmitting the electrical nerve signal down demyelinated, or damaged nerves, overwhelm the body’s ability to produce ATP ( the energy molecule). Fatigued muscles just have to stop; you feel as if you’ve run a marathon, it’s like hitting ‘the wall’ for an athlete, and you have to sit down. After a short while, energy is replenished, and you can go again.
The second type of fatigue is more of a widespread, overwhelming all-over fatigue, described here by MS campaigner, Shoshana Pezaro in 2015:
“It’s an absolutely crushing physical and mental symptom that cannot be overcome through will-power. When fatigue hits, I feel like my plug has been pulled out. Physically my body suffers extreme weakness and heaviness and every tiny movement, even raising my hand, is like fighting through thick treacle. But the mental effects are worse. The world separates from my consciousness. My brain is shrouded in a deep fog. It is a dreamlike state where I can hear people and see people, but I somehow I cannot connect. Fatigue cannot be fought, only managed through rest and care.”
Lots of research and debate has been carried out about what causes this type of fatigue; an interesting study reported at ECTRIMS conference investigated whether fatigue was more strongly linked to lesions in the brain, or to inflammation. They found a strong correlation to inflammation as the driver of this type of fatigue.
So to address Fatigue, we need to address the MS itself, and take both a short and a long view. The good thing is, there is a lot you can do to address both MS itself, and the problem of fatigue.
Starting with the most simple, here’s my list:
- Obviously read all the MS Society ( you can download here)
http://www.mssociety.org.uk/ms-resources/fatigue-ms-essentials-14 and
- MS Trust standard advice https://www.mstrust.org.uk/a-z/fatigue
pace yourself, budget your energy, and:
- Get your groceries delivered online
- Call a family meeting, explain that fatigue is a physical problem in MS, and give the family information about it, set rules and boundaries and share out the chores!

picture from http://www.goodtoknow.co.uk
- Save your energy for the stuff that counts – if you can get a cleaner, do so!
- Fluids – ensure you drink plenty of water
The Fatigue Management program, FACETs (Fatigue: Applying Cognitive behavioural and Energy effectiveness Techniques to life Style) is now available online at: https://www.mssociety.org.uk/about-ms/signs-and-symptoms/fatigue/managing-fatigue/online-fatigue-management-course
- The drug Amantadine can be tried for fatigue in MS but it only seems to help about 20% of people, and sometimes causes unpleasant side-effects
Sleep
It seems obvious, but if your sleep is poor, you will have fatigue!
Sleep problems:
- No caffeine drinks after 6pm
- Consider having something to eat before bed to prevent low blood sugar
- Try to get outside as early as possible (once the sun is up) in the day, and making sure you are outside for at least ½ an hour a day; this helps to set your body’s circadian rythm( wake-sleep cycle)
- Address causes of waking if possible – eg bladder, worrying, spasm, pain
- Consider natural sleep aids like ‘Nightall’ etc which are made from hops and valerian – check that its ok to take these with any medication you are on
- Use the HeartMath technique, for 10 minutes every morning, plus whenever you experience negative or worrying thoughts, or mind is free, and when you’re going to sleep at night.
-
Lock into a positive emotion
-
Focus on heart area
-
Breathe in for 5 seconds and out for 5 seconds in one long continuous cycle
-
imagine blowing up a balloon in your belly as you breathe in – your abdomen should rise first, then abdomen squeezes in as you expel the last bits of air out.
HeartMath is wonderful – I can’t find a good website to make it simple; you can buy all kinds of gadgets to allow yourself to see how you’re doing and coach yourself further, but the basic technique is this simple, and it has powerful and far-reaching effects on your resilience to stress, amongst other things.
Additional extras to consider.
Energy is created in our bodies by mitochondria, the ‘powerhouse’ of the cell. Each cell contains up to a thousand mitochondria. Mitochondria take fuel from the food we eat, and transform it into energy. They generate a chemical called ATP, which transports the energy for use by the body.
In order to function properly, mitochondria need the fuel of excellent nutrition and oxygen.
Dietary factors
- Everything that we put in our mouths can either be pro-inflammatory or anti-inflammatory; what we eat has an impact on inflammation.
- A study published in July 2016 showed improvements in fatigue over the course of one year, in people with MS who adopted a low fat, plant-based diet

- See www.overcomingmulstiplesclerosis.org for this type of diet, which could be expected to reduce inflammation, www.fatfreevegan.com for recipes.
- Also have a look at the work of Terry Wahls, a medical doctor who reversed her own secondary progressive MS with advanced nutrition, online. I prefer the overcomingms diet as above, but Terry’s extras like green smoothies and intense nutrition make sense to add in.
- Be aware of food intolerances. More people with MS have full blown celiac disease than in the general population, but you can also have a milder food intolerance that is not picked up by clinical allergy testing. Experiment to find out if some foods worsen your fatigue, by excluding them for 3 weeks and then bringing them in and noticing. Common irritating foods are bread, cheese, dairy products, gluten grains, sugar, and sometimes beans, but many people have individual things that they don’t tolerate.
- Vitamin D3 at least 5000 IU daily & consider minimal erythmal dose sunbed. Some people may need more to get into the optimal range of 150-200nmol per litre; you can get your blood checked at http://www.vitamindbloodtest.org.uk
- A study published this year found a significant reduction in fatigue in people with MS who took 500mg of Co-enzyme Q10 daily.
- Omega 3 fatty acids are found in oily fish, nuts, seeds and whole grains, and help to calm down and prevent inflammation, aswell as helping to store and retain energy. 20g daily can be supplied by 2 dessert spoons of cold pressed flax seed oil used cold, and make sure it’s fresh; one example; www.flaxfarm.co.uk
- B vitamins – some people are deficient in these, which can mimic symptoms of MS; some people report these help with fatigue; probably when there has been some deficiency present.
- Probiotics & fermented foods– very important to restore health of gut, especially after antibiotics, which contributes to health/ energy
- Many people report that hyperbaric oxygen improves MS fatigue; if this isn’t possible, at least do deep breathing!
- Just had great comment in response to this post by Frank:
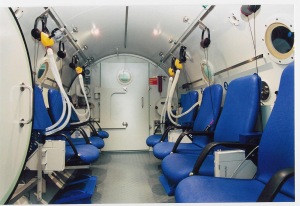
- “The very best thing for me has been taking Oxygen Therapy at the MS Centre. There are 56 centres to choose from so there’s almost bound to be one near you – unless you live in Northumberland or Cumbria.
With Oxygen Therapy and MS, lots of us find there there is an optimum pressure. The ascending protocol suggests that people should start at 1.5 ATA, move to 1.75 ATA and then try 2 ATA. After each session note down how you feel immediately afterwards and then again about 24 hours later. Once you’ve tried all three pressures you should know the one that suits you best.
As you say, Miranda, it does not work for everyone, but then neither do any of the drug or dietary therapies – we are all different – however, I’ve found it great for reducing my fatigue and if I miss my weekly session, I certainly feel the impact. Some of my colleagues find they are really tired after the Oxygen Therapy but then feel full of energy the next day, others, like myself, feel the benefit within a few hours. Whatever your views, it’s definitely worth giving it a go.” - Regular cardiovascular exercise can help to raise oxygen and energy levels, in your own zone of tolerance. Exercise has been shown to be strongly anti-inflammatory – make it part of your daily routine in one form or another.
- Some people with fatigue have reported improvement to fatigue by raising the head of their bed by 6 inches. Called ITB or inclined bed therapy – See New Pathways issue 62
APS Therapy
At the MS Therapy Centre where I work we have now had many cases of people’s MS fatigue, including post relapse, responding very well to APS Therapy. This makes sense as the treatment stimulates production of ATP, and is a replica of the wave-form of action potentials ( the electrical nerve signal.) It hasn’t worked for everyone that’s tried it; it seems to be more effecitve for fatigue in relapsing remitting, rather than progressive MS, and we are still collecting data about this, but the therapy is available privately ( see ‘my other work’ button) and at 7 MS Therapy Centres:
It hasn’t worked for everyone that’s tried it; it seems to be more effecitve for fatigue in relapsing remitting, rather than progressive MS, and we are still collecting data about this, but the therapy is available privately ( see ‘my other work’ button) and at 7 MS Therapy Centres:
Bedford, Portsmouth, Kent, Sutton & Croydon, Leicester, Berkshire and Hertfordshire and MS-UK’s Wellbeing centre, Joseph’s Court in Colchester.
Therapies
Lots of therapies, including Shiatsu, Reflexology, Yoga and ‘EFT’ tapping are found by people to improve wellbeing, energy and sleep which may then help with fatigue.
Remember that Disease Modifying Therapies (DMTs) all aim to reduce inflammation and relapses, and by doing so, can have a marked impact on reducing fatigue and improving how you feel. If you are eligible, but not on a DMT, review and reconsider the situation. If you’re on a DMT but still having relapses, request a review, as per the the MS Brain Health Campaign. And when choosing a DMT, ask about the common side-effects, explore how other people have responded, and choose one that fits best with your needs and aims.
In summary, with both long and short term strategies, there are lots of things you can do to beat fatigue and enhance your energy. Some of the long term strategies take longer to bear fruit – but keep going; many people with MS can remember a time when they were so much more fatigued than they are now.
All the best
Miranda