This blog is an article in the last issue of the excellent New Pathways MS magazine, which they have kindly allowed me to share on my blog, too!
Hello and thanks for inviting me to do a regular column with New Pathways. As an MS Nurse with an interest in integrative medicine/ holistic health, when I explore a topic here, I will generally move from the conventional advice to exploring some of the more natural approaches that may also help.
Recent interactions with one of my very young patients, got me focussing on anxiety and PANIC ATTACKS! So here goes
Panic attacks are intensely frightening events that happen when our systems are overloaded with stress hormones, causing a dry mouth, pounding heart, feeling of shortness of breath, dizziness, shaking, and sometimes, tingling ( as we hyperventilate) and chest pain. It can feel as if you’re about to die – which of course, increases the anxiety! After a nasty experience with a panic attack, it can be easy to develop a fear of having another one.
Starting with the conventional, tell your GP what’s happening. The NICE guidelines for the medical management of panic attacks recommend firstly, education and monitoring, secondly, Cognitive behavioural therapy (CBT) or relaxation therapy, and only in extreme cases that do not resolve, an anti-depressant medication, such as sertraline ( which can have the dangerous side effect of causing suicidal thoughts in a minority of people)
The NHS Website has a handy self-help guide: http://www.nhs.uk/Conditions/Panic-disorder/Pages/self%20help.aspx
I had my own experiences with panic attacks as a teenager, living abroad and drinking way too much coffee for my system, so all these suggestions come from an amalgamation of personal experience, nursing experience and learning!.
So let’s have a look at both immediate and long term strategies for mastering this problem.
If you feel one coming on:
Remember: Panic attacks aren’t dangerous. Remind yourself that it’s happening because of anxiety; your body is OK, and the very worst that could happen it that you could become dizzy from breathing too fast , and pass out, after which, your body will regulate itself again, and you’ll go back to normal. If you’re driving, pull over.
Change your focus from scary sensations, to something else that’s tangible – a sound, a feeling, a smell – part of being ‘mindful’ I found that focussing on something else – squeezing my toes and calf muscles, for instance, could distract me. Even searching for a specific item in a supermarket, or counting. Having someone chatting to you, perhaps, squeezing or massaging hands, also helps.
Regulate your breathing. Slow your breathing and count it in and out, starting with a count of three, and slowing if you can, to a count of five.
Rescue Remedy is a homeopathically diluted ( meaning that it works on an energy level, rather XX UNLIKE than like herbal or conventional medicine, and is safe to take whatever other tablets you may be on) Bach flower remedy, that many people find effective for times of crisis. See http://www.nelsonsnaturalworld.com/en-gb/uk/our-brands/rescue-remedy/the-rescue-story.There is also a spray, and pastilles; use when you feel at risk of panic attack.

Preventing further panic attacks.
Gaining mastery over our states of mind is a lifelong learning process, and something we will probably never completely perfect. However, there are ways to prevent complete overwhelm from ruling us.
Anxiety and panic attacks can be very isolating. Connecting with others and having their support defuses this feeling, so tell other people who care about you, and let them know how they can help you through.
Connecting with others and having their support defuses this feeling, so tell other people who care about you, and let them know how they can help you through.
In healthcare, we have a tendency to medicalise everything, and by doing this, we sometimes miss the obvious. It’s worth taking some time to think about the practical issues that may be causing feelings of anxiety and panic, and to ask – are there are any practical actions that can be take to make things easier? If something feels overwhelming, is there any help you can get? Can deadlines be extended? Can you get workplace support? Do you have to do things in the same way or can changes be made? Can a charity be approached to help fund an item that would help, but that you can’t afford? I often use www.Turntous.org for this. Getting organised, setting realistic goals, getting help, and taking small steps and deciding on future steps can help to restore a sense of equilibrium.
Because the hormones caused by stress are ‘burned up’ by exercise, making exercise, as much as you can, a regular part of your routine, is a powerful assistance in prevention.
Unstable blood sugar can also contribute to panic attacks, so coming off sugar and eating whole foods is helps. Coffee can cause anxiety and panic symptoms all by itself in susceptible individuals, so cut caffeinated coffee out completely.
Herbalists often recommend ‘adaptogens’ – herbs with the ability to lower stress hormones or increase resilience to stress. You can learn more at: http://nourishholisticnutrition.com/what-are-adaptogens-and-how-do-they-work/
One of the most powerful tools to become more resilient to stress and prevent anxiety and panic attacks that I have found ( through personal experience) is something called HeartMath. This is a very simple technique where you breathe in a rhythm of 5 (seconds) in, 5 out, in one continuous flow, whilst focussing on heart felt positive emotions, in the heart area. Technology can be added to allow teaching or self-monitoring using gadgets, or a sensor connected to heart rate variability display, but the basic technique is as free and as old as the hills; however, done regularly, it has the most profound effect on resilience to stress and mental, emotional and physical health. See https://mirandasmsblog.com/category/heartmath/ for my study in people with MS, and http://www.heartmath.com for more information.

Likewise, anything that helps to restore a connection to a sense of inner peace – 
meditation, deep relaxation, helps to prevent overwhelm and retain balance. You don’t need technology to meditate, but there are loads of apps available now for phones, like http://www.headspace.com. These type of things need to be done daily to build resilience to stress, to be effective.
Moving into the world of energy and its flow, certain positions help to ‘ground’ us and defuse overwhelming feelings of panic. There’s a wealth of yoga exercises that strengthen and ground, but also some quick tricks, like ‘Cook’s Hook-ups’ from Educational Kinesiology: watch this video, and do try this at home!
https://www.youtube.com/watch?v=W8Ns-2yENgc
pic (c) Maryam Webster http://maryamwebster.com/stressrelief/
It’s not always possible to take up a strange position, especially if you’re at work or on the tube for instance! But Mudras, or hand-yoga is often possible!. Mudras change the flow of energy around the body, affecting physical and mental states, and are a part of the Indian system of medicine called Ayurveda. Here’s a link to the mudras for anxiety and depression https://youtu.be/X8OgsX9b3JA.
image from http://www.stylecraze.com/articles/8-yoga-mudras-to-overcome-any-ailments/#gref
In summary, panic attacks can be caused by many factors, so having a multi-factorial approach, with patience, to achieve the goal of mastering them, makes sense. I hope these resources are useful, and if you have your own personal tips, please do share them by commenting.
All the best, Miranda











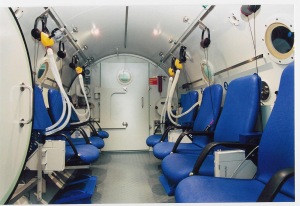
 It hasn’t worked for everyone that’s tried it; it seems to be more effecitve for fatigue in relapsing remitting, rather than progressive MS, and we are still collecting data about this, but the therapy is available privately ( see ‘my other work’ button) and at 7 MS Therapy Centres:
It hasn’t worked for everyone that’s tried it; it seems to be more effecitve for fatigue in relapsing remitting, rather than progressive MS, and we are still collecting data about this, but the therapy is available privately ( see ‘my other work’ button) and at 7 MS Therapy Centres:




 Miranda Olding, MS Specialist Nurse, England
Miranda Olding, MS Specialist Nurse, England Olding’s study included three men and 17 women from the ages of 19 and 63, all of whom “believed that stress was, or had recently been exacerbating their MS.” The patients who believed stress was a “trigger factor” for a relapse or worsening of their MS symptoms consented to participating in HeartMath training.
Olding’s study included three men and 17 women from the ages of 19 and 63, all of whom “believed that stress was, or had recently been exacerbating their MS.” The patients who believed stress was a “trigger factor” for a relapse or worsening of their MS symptoms consented to participating in HeartMath training. IHM Director of Research Rollin McCraty explains: “Heart rate variability (HRV), a measure of how responsive the heart is to tiny chemical changes in the bloodstream, stimulating the heart to beat or relax, is directly affected by emotion. Negative emotion such as frustration or anger cause a low or incoherent HRV pattern, and positive emotions such as gratitude cause a high HRV pattern.”
IHM Director of Research Rollin McCraty explains: “Heart rate variability (HRV), a measure of how responsive the heart is to tiny chemical changes in the bloodstream, stimulating the heart to beat or relax, is directly affected by emotion. Negative emotion such as frustration or anger cause a low or incoherent HRV pattern, and positive emotions such as gratitude cause a high HRV pattern.”